Covered Services
Learn more about what we cover -including health, dental, and pharmacy.
. A yearly deductible before TRICARE cost-sharing will begin: $300 per individual/$600 per family. For services beyond this deductible, you pay 50% of the TRICARE-allowable charge. These costs do not apply to the catastrophic cap. TRICARE SELECT® (JAN. 31, 2021) Includes TRICARE Select, TRICARE Overseas Program. Note: Visit our Copayment and Cost-Share Information page for 2021 costs. View the cost information below for TRICARE Reserve Select (TRS) beneficiaries. The sponsor's enlistment date does not determine costs. TRS members are covered under TRICARE Select. Benefits, cost-shares and deductibles are the same as Group B active duty family members.
On Jan. 1, some copayments for your prescription drugs will increase. If you get your prescriptions through the TRICARE Pharmacy Home Delivery or at a retail network pharmacy, you’ll pay anywhere from $2 to $7 more starting Jan. 1. Congress made this change in the National Defense Authorization Act for Fiscal YearOctober 1 - September 30 2018.
There’s still no cost to fill your prescriptions at military pharmacies. And these cost changes don’t apply to active duty service members (ADSMs). If you’re an ADSM, you still pay nothing for your covered drugs at military and network pharmacies.
“Military pharmacies remain to be your lowest cost option,” said U.S. Air Force Lt. Col. Melissa Pammer with the Pharmacy Operations Division at the Defense Health Agency. “Your next lowest cost is if you use the TRICARE Pharmacy Home Delivery.”
TRICARE Prescription Drug Categories
Your prescription copayments vary based on pharmacy type. Also, they vary based on the drug category. TRICARE groups prescription drugs into one of four categories. This grouping is based on the medical and cost effectiveness of a drug compared to other drugs of the same type.
As outlined in the TRICARE Pharmacy Program Handbook, the drug categories include:
- Generic formulary drugs: These drugs are widely available. You have the lowest out-of-pocket costs for these drugs.
- Brand-name formulary drugs: These drugs are generally available to you. Plus, they offer you the second lowest copaymentA fixed dollar amount you may pay for a covered health care service or drug..
- Non-formulary drugsA drug in a therapeutic class that isn’t as clinically or cost-effective as other drugs in the same class. You pay a higher cost share for these drugs.: These drugs may have limited availability. You have higher copayments for these drugs. Also, there’s generally an alternative formulary drug that you can get. It’s often more cost effective, and equally or more clinically effective.
- Non-covered drugs: TRICARE doesn’t cover these drugs. If you choose to purchase a non-covered drug, you’ll pay 100% of the drug’s cost. These drugs are either not clinically effective, or as cost effective as other drugs offered. They may also pose a significant safety risk that may outweigh any potential clinical benefit.
To learn more, you can download the TRICARE Pharmacy Program Handbook from the Publications page.
Pharmacy Copayment Increases
TRICARE Pharmacy Home Delivery
If you use home delivery, your copayments for up to a 90-day supply of generic formulary drugs will increase from $7 to $10. For brand-name formulary drugs, your copayments will increase from $24 to $29. Your copayments for non-formulary drugs when you don’t have a medical necessity will increase from $53 to $60.
TRICARE retail network pharmacies
At a retail network pharmacy, your copayments for up to a 30-day supply of generic formulary drugs will increase from $11 to $13. For brand-name formulary drugs, the increase is from $28 to $33. Non-formulary drugs will increase from $53 to $60.
Non-network pharmacies
At a non-network pharmacy, you must pay the full price of the drug. After meeting your annual deductible, you may submit a claim for partial reimbursement. Non-network pharmacy costs remain the same if you use TRICARE Prime. With TRICARE Prime, you’ll pay a 50% cost-shareA percentage of the total cost of a covered health care service that you pay. after meeting your point-of-service deductible for covered drugs.
For all other health plans, non-network pharmacy costs are as follows:
- Generic formulary drugs and brand-name formulary drugs will cost $33 (up from $28) or 20% of the total cost, whichever is more, after you meet your annual deductible.
- Non-formulary drugs will cost $60 (up from $53) or 20% of the total cost, whichever is more, after you meet your annual deductible.
Copayments for survivors of ADSMs are the same as the 2017 rates. The copayments remain the same for medically retired service members and their family members, too.
For the latest TRICARE pharmacy costs, you should visit TRICARE Costs. To learn more about your pharmacy benefit, visit Pharmacy on the TRICARE website.
Last Updated 2/17/2021
Covered Services
Learn more about what we cover -including health, dental, and pharmacy.
UPDATE: There’s new information available regarding TRICARE Select enrollment fees. Visit www.tricare.mil/selectenrollmentfees to learn more.
Starting on Jan. 1, 2021, TRICARE Select Group A retired beneficiaries must pay monthly enrollment fees in order to maintain their TRICARE health coverage. This is a change, and the first time this beneficiary group will pay enrollment fees.
Tricare Reserve Select Copay 2021
“In 2021, some TRICARE beneficiaries will pay enrollment fees for the first time, a change mandated by Congress,” said Dr. Danita Hunter, director of the TRICARE Health Plan at the Defense Health Agency. “We’re communicating this well before the change is implemented so beneficiaries can be informed about the change, as well as their TRICARE plan and cost options.”
Here are the key points you need to know.
What’s happening?
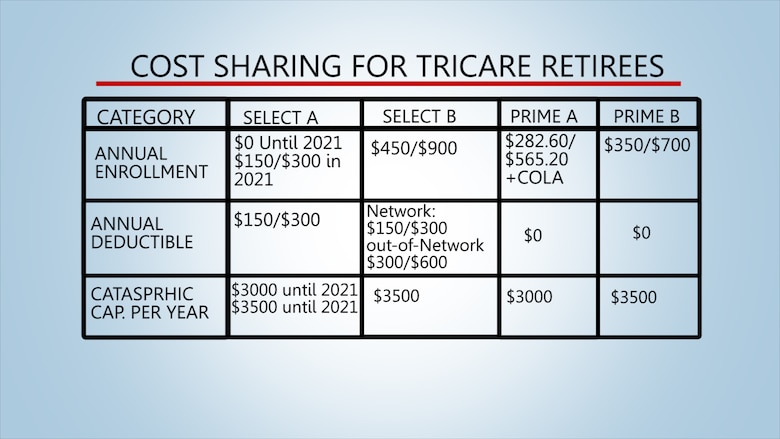
Retired TRICARE Select beneficiaries will have to pay enrollment fees. This change was mandated by Congress in the National Defense Authorization Act for Fiscal YearOctober 1 - September 30 2017. Congress granted the Defense Health Agency a delay in implementation to calendar year 2021.
Who’s impacted?
This change only affects Group AIf you or your sponsor’s initial enlistment or appointment occurred before January 1, 2018, you are in Group A. retirees and their family members enrolled in TRICARE Select. You’re in Group A if your initial enlistment or appointment or that of your uniformed services sponsor began before Jan. 1, 2018. Active duty family members enrolled in TRICARE Select will experience no change, and won’t pay enrollment fees.
If you use TRICARE For Life, TRICARE Prime, or a premium-based plan, like TRICARE Reserve Select, TRICARE Retired Reserve, or TRICARE Young Adult, this change won’t affect you. To check your plan’s costs, use the TRICARE Compare Cost Tool.
This applies to me. When do I need to take action?
You must contact your TRICARE regional contractor to set up a monthly allotment withdrawn from your Department of Defense (DoD) pay center, where feasible, for your monthly payments to start on Jan. 1, 2021. Don't try to create an allotment directly through your pay center. For sponsors who don’t receive funds through a DoD pay center, you can establish payments via electronic funds transfer, credit card, or debit card.
What are the 2021 enrollment fees for TRICARE Select Group A retirees?
Tricare Pharmacy Copay 2021

The enrollment fees will be collected via monthly installments from the sponsor’s military pay system where retired pay is disbursed.
- Individual plan: $12.50 per month
- Family plan: $25 per month
How can I stay informed and prepare for this change?
Visit the TRICARE Select Enrollment Fees page on the TRICARE website for updates and sign up for email alerts. TRICARE will inform you of specific actions you need to take in the coming months. Take command of your health and your health care benefits in 2020.

Last Updated 2/17/2021
